A New OD's Guide to Fitting Rose K RGP Lenses for Irregular Corneas
3:07 PMWhether your patient has keratoconus, pellucid marginal degeneration, or irregular cornea post-corneal graft surgery, standard contact lens solutions are likely not going to provide the best vision. While scleral lenses have become a go-to for irregular corneas over the past decade, some patients struggle with insertion and removal of a larger lens, and a smaller RGP option is more ideal for them. Luckily the ROSE K family of RGP lenses gives us a range of options and is available from a number of different specialty contact lens manufacturers across multiple countries.
I highly encourage you to visit the ROSE K practitioner website for in depth fitting guides, FAQs, and even videos. But if you are looking for a quick beginner's reference guide for getting started with this lens, this post is for you!
ROSE K lens selection
For each type of irregular cornea, well there's a Rose K lens for that. Each fit set has different fitting protocols for selecting initial lens base curve, so the first important step to a good Rose K fit is to choose the right fit set for your patient.
Rose K2 KC: for keratoconus patients and more oval cones - most of your keratoconus fits (around 70%) will use this lens
Rose K2 NC: for keratoconus patients with very central "nipple" cones. This is where the center of the cone is within 1 mm of the visual axis
Rose K2 PG: for post-graft patients with more oblate corneas
Rose K2 IC: for more diffuse irregular corneas like pellucid marginal degeneration patients
Rose K2 XL: a corneoscleral lens for larger diameter irregularities
Rose K2 Oblate XL: a corneoscleral lens for larger diameter irregularities post-surgical oblate corneas
Most of the irregular corneas a practitioner will be fitting are keratoconus patients, and most keratoconus patients would fall under the Rose K2 KC lens so that's likely the fit set you'll use most. I say this as a practitioner that only has the Rose K2 IC fit set and have wondered why the base curve fitting guide always seems to be wrong for me - after further education I know now it's because I was trying to fit a lens design that wasn't made for this specific patient group. Don't make my mistake - use the right fit set for the right patient category.
 |
| via |
ROSE K FUNDAMENTALS OF A GOOD FIT
There are 5 steps to a good Rose K fit - after you've selected the right fit set for the patient you have in front of you of course.
1. Central Fit - base curve selection
Follow the fit guide for how to convert your patients K readings to initial diagnostic lens selection. Place the lens on eye and instill NaFL dye to assess the pattern. You only need to wait a minute or so for settling - the lens will reveal how it fits very quickly. Judge the fit relationship immediately after a blink. Look for a "light feather touch" over the steepest apex of the cornea. What is a light feather touch? If you go just 0.1 mm steeper, then you'll get no touch. Bracketing the fit steeper and flatter until you find that point of just barely touch is ideal.
What happens if you fit a lens too flat (with more than a "light feather touch")? If the lens is rubbing on the cornea you can create punctate keratitis or even scarring issues. The lens will be uncomfortable or even painful to wear.
If you fit a lens too steep (too far off the cornea) you will get vision issues with halos, ghosting, and fluctuating vision. You can even have "dimple veiling" on the cornea where bubbles under the too-steep lens cause distortion to the corneal surface.
Both too flat and too steep cause problems, so it's important to spend extra time getting that initial base curve selection nailed down by bracketing until you find the most ideal lens fit where just 1 step steeper is too steep.
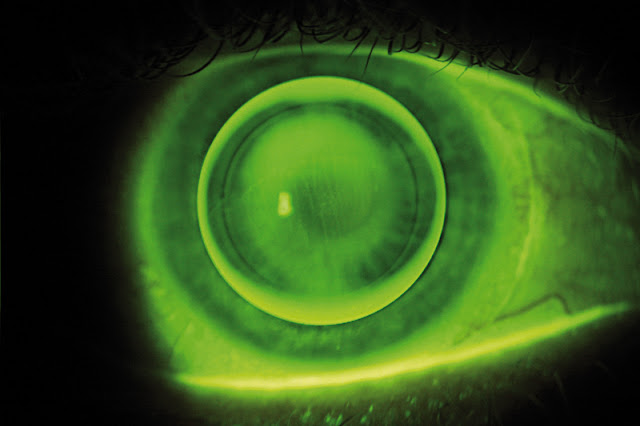 |
| A "light feather touch" over the apex of the cone is ideal. via |
 |
| this fit is too flat - need to increase the base curve! via |
2. Peripheral Fit - edge selection
All of the diagnostic lenses in your fit set come with a standard edge lift. When evaluating the lens edge focus on the 3 + 9 o'clock position because that is usually the flattest meridian of the cornea. Ideally you should see 0.6-0.8 mm band of NaFL dye at the edge. If the edge is too tight (barely any NaFL dye) then increase the edge lift to flatten the periphery. If the edge is too loose (excessive NaFL dye) then decrease the edge lift to steepen the periphery. A loose edge your patient will tell you how uncomfortable it is!
3. Overall Diameter
Per fitting gurus you want "the smallest diameter needed for good centration and movement". The larger the irregularity of the cornea, the larger your diameter will need to be. A central nipple cone patient will need a smaller diameter lens; a patient with pellucid where the irregularity is really far from the visual axis will need a larger diameter lens.
Your diagnostic lens set comes in specific diameter ranges for each type. So for example the Rose K NC has much smaller diameter than the Rose K PG where the irregularity would be more peripheral. This takes us back to the original point where you need to pick the right Rose K fit set for the type of patient you are fitting.
4. Location - is the lens centered?
You can adjust lens centration by adjusting 1) edge lift, 2) base curve, and 3) diameter. Make adjustments in that order until each element is maximized to ideal fit relation as outlined above.
If a lens is riding high:
- Decrease the edge lift
- Steepen the base curve
- Decrease the diameter
If a lens is riding low:
- Increase the edge lift
- Flatten the base curve
- Increase the diameter
 |
| This is a really great lens to troubleshoot. Obviously it is riding low. At first glance you might think there is excessive edge lift, BUT remember you should judge edge lift and 3+9. At 3+9 you actually see there is minimal edge lift, so our initial change to fix this lens centration issue would be step 1 on the guide above: increase edge lift. via |
5. Lens Movement
Movement is important for tear exchange under the lens and healthy oxygen flow to the cornea, but excessive movement can also lead to discomfort and lenses easily decentering or even falling out. Ideal lens movement is 1-2 mm with blink. Edge lift is the main element that controls movement.
Increase edge lift to increase movement; decrease edge lift to decrease movement
If a patient tells you the lens is very hard to remove and is "tight" on the eye - that's a sign to increase the edge lift.
Check out the Rose K practitioner website for more great education! And don't forget that your reps in the consultation department are skilled at troubleshooting these lenses and can help guide you in what questions to ask yourself when designing changes to a fit.















_SAND.jpg)
0 comments